脱水
| 脱水 | |
|---|---|
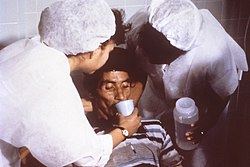 | |
| 护理师正鼓励病人喝口服补液盐来治疗霍乱引起的脱水。 | |
| 症状 | 口渴、疲倦、尿量减少、头晕、头痛及精神错乱[1] |
| 并发症 | 低血容性休克、昏迷、癫痫、泌尿道感染、肾脏疾病、中暑、高钠血症、代谢性疾病[1]、高血压[2] |
| 病因 | 体内水分流失 |
| 风险因素 | 身体缺水、热浪、疾病(最常见的是引起呕吐和/或腹泻的疾病)、运动 |
| 治疗 | 饮用干净的水 |
| 药物 | 生理盐水 |
| 分类和外部资源 | |
| 医学专科 | 重症医学 |
| ICD-11 | 5C70.0 |
| ICD-10 | E86 |
| DiseasesDB | 3520 |
| MedlinePlus | 000982 |
| eMedicine | 801012 |
脱水(英语:dehydration)在生理学上是指身体水含量不足而扰乱新陈代谢[3]。当自由水分流失超过摄取量时就会发生这种情况,通常是由于出汗过多、健康状况或饮水不足造成的。浸泡利尿也可能导致轻度脱水,并可能会增加潜水员出现减压症的风险。
大多数人可以忍受体内水分总量减少 3-4%,而不会出现任何困难或对健康产生不利影响。下降5-8%就会引起疲劳和头晕。身体整体水流失超过10%就会引起身体和精神衰退,伴随严重口渴。当体内水分流失15%到25%时就会导致死亡[4]。轻度脱水通常可以透过口服补液来解决,但严重的情况下可能需要静脉输液。
脱水会导致高钠血症(血液中钠离子含量高)。这与血容量减少(血容量损失,尤其是血浆损失)不同。
征兆和症状
[编辑]脱水的症状包括口渴和神经系统变化,如头痛、全身不适、食欲不振、恶心、尿量减少(除非多尿症是脱水的原因)、意识模糊、不明原因的疲倦、指甲发紫和癫痫。[7]随着全身失水量的增加,脱水症状会变得越来越严重。体内失水 1-2%,即为轻度脱水,会损害认知能力[8]。虽然对于 50 岁以上的人来说,身体的口渴感会随着年龄的增长而减弱,但一项研究发现,年轻人和老年人的液体摄取量没有差异[9]。许多老年人都有脱水症状,最常见的是疲劳[10]。脱水亦是老年人口身体状况较差的原因之一,尤其是在炎热天气等导致水分毫无意识地经表皮流失的情况下。
原因
[编辑]脱水的风险因子包括但不限于:在炎热潮湿的天气中劳动、居住在高海拔地区、耐力运动、老年人、婴儿、儿童和长期病患者。[11][12][13][14]
脱水也可能是多种药物的副作用。[15]
对于老年人来说,对口渴的反应迟钝或面对过多的自由水损失(尤其是高血糖相关的损失)时获取自由水的能力不足似乎是脱水的主要原因。[16]过量的自由水或低渗透压水可以透过两种方式离开人体-显性失水,如渗透性利尿、出汗、呕吐和腹泻,以及不显性失水,主要透过皮肤和呼吸道发生。在人类中,脱水可能是由多种疾病和损害体内水分平衡的状态引起的。这些情况主要由于口渴或缺水或钠过量而发生。[17]
其他引致身体脱水的原因包括:
分类
[编辑]按照钠和水丢失的比例,可以分为等渗性脱水、低渗性脱水和高渗性脱水三种。
低渗性脱水,也可称为低容量性低钠血症,特点是失钠多于失水,血清钠浓度<130mmol/L,血浆渗透压<280mmol/L,伴有细胞外液量的减少。 高渗性脱水,又称为低容量性高钠血症,特点是失水多于失钠,血清钠浓度>150mmol/L,血浆渗透压>310mmol/L,细胞外液量和细胞内液量均减少。
等渗性脱水,特点是水钠成比例丢失,血容量减少,但血清钠浓度和血浆渗透压仍在正常范围。单纯性的等渗性脱水临床上较少见。
机制
[编辑]人体含水量各不相同,新生儿体内含水量为 70-75%,肥胖成人体内含水量为 40% 甚至更低[18] ,建议平均值为 60%[19]。在体内,水被分为细胞内液或细胞外液。细胞内液是指细胞内所含的水。这约占身体水分总量的57%[18]。细胞内液含有高浓度的钾、镁、磷酸盐和蛋白质[20]。细胞外液由细胞外的所有液体组成,包括血液和组织液。这约占身体水分总量的43%。细胞外液中最常见的离子包括钠、氯和碳酸氢盐。
液体中溶解分子和离子的浓度被描述为渗透压,以每升渗透摩尔 (Osm/L) 为单位[20]。当身体缺乏自由水时,溶质的浓度就会增加。这会导致更高的血清渗透压。当血清渗透压升高时,下丘脑的渗透压感受器可以被侦测到。这些受体会引发抗利尿激素的释放[21]。抗利尿激素会透过增加肾脏的水分吸收和收缩血管来抵抗脱水。它作用于肾单位集合管细胞中的V2 受体,增加水通道蛋白的表达。在更极端的低血压情况下,下丘脑会释放大量抗利尿激素,这也会作用于 V1 受体[22]。这些受体会引起周边血管平滑肌收缩。这会增加全身血管阻力并升高血压。
诊断
[编辑]定义
[编辑]当摄取的水无法补充因正常生理过程(包括呼吸、排尿、出汗)或腹泻、呕吐等其他原因而流失的自由水时,就会发生脱水。脱水严重时可能危及生命,导致癫痫或呼吸停止;如果保湿过快,还存在渗透性脑水肿的风险。
“脱水”一词有时被错误地用作与血容量减少有关的单独病症的替代,血容量减少具体指血浆量的减少[3]。在人类中,这两者透过独立的机制进行调节[3];这种差异对于指导治疗具有重要意义。[24]
身体检查
[编辑]脱水的常见检查结果包括黏膜干燥、腋窝干燥、毛细血管再充盈时间增加、眼睛凹陷和皮肤弹性差[25][10]。更严重的脱水状况会导致直立性低血压、头晕、虚弱和精神状态改变[26]。根据脱水的根本原因,也可能出现其他症状。运动时出汗过多可能会引起肌肉痉挛。呕吐或腹泻导致胃肠道失水的患者也可能出现发烧或其他全身性感染症状。
皮肤弹性测试可用于支持脱水的诊断。皮肤弹性测试是透过捏住患者身体上某个部位的皮肤(例如前臂或手背)并观察其恢复正常位置的速度来进行的。对于皮肤弹性降低的患者(例如老年人),皮肤弹性测试未必可靠[27]。
临床测试
[编辑]虽然没有单一的黄金标准测试来诊断脱水,但可以在涉及血液和尿液的多项实验室测试中看到证据。血清渗透压高于 295 mOsm/kg 通常见于因自由水流失而导致的脱水[10]。尿液分析是一种对尿液进行化学和微观分析的测试,透过分析可以发现严重脱水时尿液颜色会变深或发出恶臭[28]。尿钠含量也能提供有关脱水类型的信息。对于低钠性脱水,例如呕吐或腹泻引起的,尿钠将低于 10 mmol/L,因为肾脏为了保存水分而增加钠的保留[29] 。因利尿剂或肾功能不全造成钠流失的脱水患者,尿钠可能升高至20mmol/L以上[30]。患者血清尿素氮和肌酸酐浓度也可能升高。这两种分子通常由肾脏排泄,但当循环血量低时,肾脏就会受损[31]。这会导致肾功能下降,并导致血清中尿素氮和肌酸酐升高[32]。
预防
[编辑]对于日常活动来说,口渴通常是保持适当水分的充分指导[33]。最低水摄取量因体重、能量消耗、年龄、性别、体力活动、环境、饮食和遗传等因素而异[34][35]。运动、暴露于热环境或对口渴反应降低时,可能需要补充额外的水。对于参加比赛的运动员来说,尽管体重减轻,但口渴后才喝水仍可优化运动表现和安全性,而且截至 2010 年,尚无科学研究表明在运动期间预防口渴并维持体重是有益的[36]。
在温暖或潮湿的天气,或剧烈运动时,水分流失会显著增加,因为人体出汗的能力很强,而且变化很大。在竞技运动中,男性全身出汗量每小时可超过 2 升,而在高温下进行短时间、高强度运动时,全身出汗量则为 3-4 升/小时[37]。当大量的水分经由流汗流失时,电解质,特别是钠,也会流失[38]。
对于大多数运动员来说,运动并出汗 4-5 小时(而汗液钠浓度低于 50 mmol/L),总钠流失量不到身体总储量的 10%(总储量约为 2,500 mmol,对于一个 70 公斤的人来说为 58 克)[39]。大多数人似乎都能很好地承受这些损失。在补液饮料中添加钠在理论上有一些好处[39],而且只要这些液体是低渗透压的(因为预防脱水的主要方法是补充自由水的损失),就不会带来任何风险。
治疗
[编辑]一般认为,轻度脱水最有效的治疗方法是喝水和减少体液流失。白开水只能恢复血浆的量,在溶质水平补充之前会抑制口渴机制[40]。食用固体食物也有助于补充水分。据估计,美国人摄取的水量约有 22% 来自食物[41]。随着脱水症状消退,尿液浓度和小便频率将恢复正常[42]。
在某些情况下,透过补充必要的水分和电解质(透过口服补液疗法或静脉输液疗法)来纠正脱水状态。由于口服补液痛苦较小、非侵入性、价格低廉且更容易提供,因此它是轻度脱水的首选治疗方法[43]。用于静脉补液的溶液可能是等渗透压的、高渗透压的或低渗透压的,这取决于脱水的原因以及血液中的钠浓度[44]。注射纯净水至静脉会导致红血球的分解(溶解)[45]。
当无法取得淡水时(例如在海上或沙漠中),海水或酒精浓度较高的饮料会加剧脱水情况。尿液中溶质的浓度比海水低;这需要肾脏产生更多的尿液来去除多余的盐分,导致流失的水分比从海水中吸收的水分还要多[46]。如果病人脱水并被送往医疗机构,也可以使用静脉注射[47]。
对于严重脱水病例,出现昏厥、昏迷或其他严重抑制症状(患者无法直立或清晰思考),需要紧急治疗。口服或静脉注射含有适当平衡的替代电解质的液体,并持续评估电解质状态;除最极端的情况外,严重脱水的症状通常可以完全解决[48]。
预后
[编辑]脱水的预后取决于脱水的原因和程度。轻度脱水通常可以透过口服补液来解决。慢性脱水,例如因体力劳动或口渴减少而引起的脱水,可能导致慢性肾脏病[49]。脱水的老人出现精神错乱、泌尿道感染、跌倒,甚至伤口愈合延迟的风险更高[50]。对于轻度至中度脱水的儿童,口服补液足以使其完全康复[51]。
参见
[编辑]外部链接
[编辑]- 夏日喝太多水 恐“中毒”致命
- Definition of dehydration by the U.S. National Institutes of Health's MedlinePlus medical encyclopedia (页面存档备份,存于互联网档案馆)
- Rehydration Project at rehydrate.org (页面存档备份,存于互联网档案馆)
- Steiner, MJ; DeWalt, DA; Byerley JS. Is this child dehydrated?. JAMA: the Journal of the American Medical Association. Jun 9, 2004, 291 (22): 2746–54. PMID 15187057. doi:10.1001/jama.291.22.2746.
参考资料
[编辑]- ^ 1.0 1.1 Dehydration - Symptoms and causes. Mayo Clinic.
- ^ El-Sharkawy AM, Sahota O, Lobo DN. Acute and chronic effects of hydration status on health. Nutrition Reviews. September 2015, 73 (Suppl 2): 97–109. PMID 26290295. doi:10.1093/nutrit/nuv038.
- ^ 3.0 3.1 3.2 Mange K, Matsuura D, Cizman B, Soto H, Ziyadeh FN, Goldfarb S, Neilson EG. Language guiding therapy: the case of dehydration versus volume depletion. Annals of Internal Medicine. November 1997, 127 (9): 848–853. PMID 9382413. S2CID 29854540. doi:10.7326/0003-4819-127-9-199711010-00020.
- ^ Ashcroft F, Life Without Water in Life at the Extremes. Berkeley and Los Angeles, 2000, 134-138.
- ^ Seal AD, Suh HG, Jansen LT, Summers LG, Kavouras SA. Hydration and Health. Pounis G (编). Analysis in Nutrition Research. Elsevier. 2019: 299–319. ISBN 978-0-12-814556-2. doi:10.1016/b978-0-12-814556-2.00011-7 (英语).
- ^ Clark WF, Sontrop JM, Huang SH, Moist L, Bouby N, Bankir L. Hydration and Chronic Kidney Disease Progression: A Critical Review of the Evidence. American Journal of Nephrology. 2016, 43 (4): 281–292. PMID 27161565. doi:10.1159/000445959
 .
.
- ^ The Handbook Of The SAS And Elite Forces. How The Professionals Fight And Win. Edited by Jon E. Lewis. p.426-Tactics And Techniques, Survival. Robinson Publishing Ltd 1997. ISBN 1-85487-675-9
- ^ Riebl SK, Davy BM. The Hydration Equation: Update on Water Balance and Cognitive Performance. ACSM's Health & Fitness Journal. November 2013, 17 (6): 21–28. PMC 4207053
 . PMID 25346594. doi:10.1249/FIT.0b013e3182a9570f.
. PMID 25346594. doi:10.1249/FIT.0b013e3182a9570f.
- ^ Hall H. Are You Dehydrated?. Skeptical Inquirer. August 17, 2020, 4 (4).
- ^ 10.0 10.1 10.2 Hooper L, Abdelhamid A, Attreed NJ, Campbell WW, Channell AM, Chassagne P, Culp KR, Fletcher SJ, Fortes MB, Fuller N, Gaspar PM, Gilbert DJ, Heathcote AC, Kafri MW, Kajii F, Lindner G, Mack GW, Mentes JC, Merlani P, Needham RA, Olde Rikkert MG, Perren A, Powers J, Ranson SC, Ritz P, Rowat AM, Sjöstrand F, Smith AC, Stookey JJ, Stotts NA, Thomas DR, Vivanti A, Wakefield BJ, Waldréus N, Walsh NP, Ward S, Potter JF, Hunter P. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. The Cochrane Database of Systematic Reviews. April 2015, 2015 (4): CD009647. PMC 7097739
 . PMID 25924806. doi:10.1002/14651858.CD009647.pub2. hdl:2066/110560
. PMID 25924806. doi:10.1002/14651858.CD009647.pub2. hdl:2066/110560  .
.
- ^ Paulis, Simone J. C.; Everink, Irma H. J.; Halfens, Ruud J. G.; Lohrmann, Christa; Schols, Jos M. G. A. Prevalence and Risk Factors of Dehydration Among Nursing Home Residents: A Systematic Review. Journal of the American Medical Directors Association. 2018-08-01, 19 (8): 646–657. ISSN 1525-8610. PMID 30056949. doi:10.1016/j.jamda.2018.05.009.
- ^ Sawka, Michael N; Montain, Scott J. Fluid and electrolyte supplementation for exercise heat stress1234. The American Journal of Clinical Nutrition. NIH Workshop on the Role of Dietary Supplements for Physically Active People. 2000-08-01, 72 (2): 564S–572S. ISSN 0002-9165. doi:10.1093/ajcn/72.2.564S.
- ^ Steiner, Michael J.; DeWalt, Darren A.; Byerley, Julie S. Is This Child Dehydrated?. JAMA. 2004-06-09, 291 (22): 2746–2754. ISSN 0098-7484. PMID 15187057. doi:10.1001/jama.291.22.2746.
- ^ Research, Institute of Medicine (US) Committee on Military Nutrition; Marriott, Bernadette M.; Carlson, Sydne J., Fluid Metabolism at High Altitudes, Nutritional Needs In Cold And In High-Altitude Environments: Applications for Military Personnel in Field Operations (National Academies Press (US)), 1996 [2024-11-15] (英语)
- ^ Puga, Ana M.; Lopez-Oliva, Sara; Trives, Carmen; Partearroyo, Teresa; Varela-Moreiras, Gregorio. Effects of Drugs and Excipients on Hydration Status. Nutrients. 2019-03-20, 11 (3): 669. ISSN 2072-6643. PMC 6470661
 . PMID 30897748. doi:10.3390/nu11030669
. PMID 30897748. doi:10.3390/nu11030669  (英语).
(英语).
- ^ Borra SI, Beredo R, Kleinfeld M. Hypernatremia in the aging: causes, manifestations, and outcome. Journal of the National Medical Association. March 1995, 87 (3): 220–224. PMC 2607819
 . PMID 7731073.
. PMID 7731073.
- ^ Lindner G, Funk GC. Hypernatremia in critically ill patients. Journal of Critical Care. April 2013, 28 (2): 216.e11–216.e20. PMID 22762930. doi:10.1016/j.jcrc.2012.05.001.
- ^ 18.0 18.1 Schoeller 2005,第35页.
- ^ Kamel KS, Halperin ML. Fluid, electrolyte, and acid-base physiology: a problem-based approach Fifth. Philadelphia, PA: Elsevier. 2017. ISBN 978-0-323-35515-5.
- ^ 20.0 20.1 Garden J, Parks R, Wigmore S. Principles and Practice of Surgery 8th. Elsevier Limited. 2023: 32–55. ISBN 978-0-7020-8251-1.
- ^ White BA, Harrison JR, Mehlmann LM. Endocrine and reproductive physiology. Mosby physiology series 5th. St. Louis, MI: Elsevier. 2019. ISBN 978-0-323-59573-5.
- ^ Webb AJ, Seisa MO, Nayfeh T, Wieruszewski PM, Nei SD, Smischney NJ. Vasopressin in vasoplegic shock: A systematic review. World Journal of Critical Care Medicine. December 2020, 9 (5): 88–98. PMC 7754532
 . PMID 33384951. doi:10.5492/wjccm.v9.i5.88
. PMID 33384951. doi:10.5492/wjccm.v9.i5.88  .
.
- ^ UOTW#59 - Ultrasound of the Week. Ultrasound of the Week. 23 September 2015 [27 May 2017].
- ^ Bhave G, Neilson EG. Volume depletion versus dehydration: how understanding the difference can guide therapy. American Journal of Kidney Diseases. August 2011, 58 (2): 302–309. PMC 4096820
 . PMID 21705120. doi:10.1053/j.ajkd.2011.02.395.
. PMID 21705120. doi:10.1053/j.ajkd.2011.02.395.
- ^ Huffman GB. Establishing a Bedside Diagnosis of Hypovolemia. American Family Physician. 1999-09-15, 60 (4): 1220–1225 (美国英语).
- ^ Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and Management of Sodium Disorders: Hyponatremia and Hypernatremia. American Family Physician. 2015-03-01, 91 (5): 299–307. PMID 25822386 (美国英语).
- ^ Thomas J, Monaghan T. Oxford Handbook of Clinical Examination and Practical Skills. Oxford University Press. 2014. ISBN 978-0-19-959397-2 (英语).
- ^ Hughes G. A medication guide to internal medicine tests and procedures First. Philadelphia: Elsevier, Inc. 2021. ISBN 978-0-323-79007-9.
- ^ Tietze, Karen J., Review of Laboratory and Diagnostic Tests, Clinical Skills for Pharmacists (Elsevier), 2012: 86–122 [2024-11-06], ISBN 978-0-323-07738-5, doi:10.1016/b978-0-323-07738-5.10005-5 (英语)
- ^ Yun, Giae; Baek, Seon Ha; Kim, Sejoong. Evaluation and management of hypernatremia in adults: clinical perspectives. The Korean Journal of Internal Medicine. 2023-05-01, 38 (3): 290–302. ISSN 1226-3303. PMC 10175862
 . PMID 36578134. doi:10.3904/kjim.2022.346 (英语).
. PMID 36578134. doi:10.3904/kjim.2022.346 (英语).
- ^ Mohamed, Mohamed Saied; Martin, Andrew. Acute kidney injury in critical care. Anaesthesia & Intensive Care Medicine. May 2024, 25 (5): 308–315. doi:10.1016/j.mpaic.2024.03.008 (英语).
- ^ Amin, Rasheda; Ahn, Sun-Young; Moudgil, Asha, Kidney and urinary tract disorders, Biochemical and Molecular Basis of Pediatric Disease (Elsevier), 2021: 167–228 [2024-11-06], ISBN 978-0-12-817962-8, doi:10.1016/b978-0-12-817962-8.00010-x (英语)
- ^ Institute of Medicine; Food Nutrition Board. Dietary Reference Intakes: Water, Potassium, Sodium, Chloride, and Sulfate : Health and Medicine Division. National Academies Press. June 18, 2005 [2018-02-07]. ISBN 9780309091695 (英语).
- ^ Armstrong, Lawrence E.; Johnson, Evan C. Water Intake, Water Balance, and the Elusive Daily Water Requirement. Nutrients. 2018-12-05, 10 (12): 1928. ISSN 2072-6643. PMC 6315424
 . PMID 30563134. doi:10.3390/nu10121928
. PMID 30563134. doi:10.3390/nu10121928  (英语).
(英语).
- ^ Yamada Y, Zhang X, Henderson ME, Sagayama H, Pontzer H, Watanabe D, Yoshida T, Kimura M, Ainslie PN, Andersen LF, Anderson LJ, Arab L, Baddou I, Bedu-Addo K, Blaak EE, Blanc S, Bonomi AG, Bouten CV, Bovet P, Buchowski MS, Butte NF, Camps SG, Close GL, Cooper JA, Cooper R, Das SK, Dugas LR, Eaton S, Ekelund U, Entringer S, Forrester T, Fudge BW, Goris AH, Gurven M, Halsey LG, Hambly C, El Hamdouchi A, Hoos MB, Hu S, Joonas N, Joosen AM, Katzmarzyk P, Kempen KP, Kraus WE, Kriengsinyos W, Kushner RF, Lambert EV, Leonard WR, Lessan N, Martin CK, Medin AC, Meijer EP, Morehen JC, Morton JP, Neuhouser ML, Nicklas TA, Ojiambo RM, Pietiläinen KH, Pitsiladis YP, Plange-Rhule J, Plasqui G, Prentice RL, Rabinovich RA, Racette SB, Raichlen DA, Ravussin E, Redman LM, Reilly JJ, Reynolds RM, Roberts SB, Schuit AJ, Sardinha LB, Silva AM, Sjödin AM, Stice E, Urlacher SS, Valenti G, Van Etten LM, Van Mil EA, Wells JC, Wilson G, Wood BM, Yanovski JA, Murphy-Alford AJ, Loechl CU, Luke AH, Rood J, Westerterp KR, Wong WW, Miyachi M, Schoeller DA, Speakman JR. Variation in human water turnover associated with environmental and lifestyle factors. Science. November 2022, 378 (6622): 909–915. Bibcode:2022Sci...378..909I. PMC 9764345
 . PMID 36423296. doi:10.1126/science.abm8668.
. PMID 36423296. doi:10.1126/science.abm8668.
- ^ Noakes TD. Is drinking to thirst optimum?. Annals of Nutrition & Metabolism. 2010, 57 (Suppl 2): 9–17. PMID 21346332. doi:10.1159/000322697
 .
.
- ^ Taylor NA, Machado-Moreira CA. Regional variations in transepidermal water loss, eccrine sweat gland density, sweat secretion rates and electrolyte composition in resting and exercising humans. Extreme Physiology & Medicine. February 2013, 2 (1): 4. PMC 3710196
 . PMID 23849497. doi:10.1186/2046-7648-2-4
. PMID 23849497. doi:10.1186/2046-7648-2-4  .
.
- ^ Baker, Lindsay B. Sweating Rate and Sweat Sodium Concentration in Athletes: A Review of Methodology and Intra/Interindividual Variability. Sports Medicine. March 2017, 47 (S1): 111–128. ISSN 0112-1642. PMC 5371639
 . PMID 28332116. doi:10.1007/s40279-017-0691-5 (英语).
. PMID 28332116. doi:10.1007/s40279-017-0691-5 (英语).
- ^ 39.0 39.1 Coyle EF. Fluid and fuel intake during exercise. Journal of Sports Sciences. January 2004, 22 (1): 39–55. CiteSeerX 10.1.1.321.6991
 . PMID 14971432. S2CID 14693195. doi:10.1080/0264041031000140545.
. PMID 14971432. S2CID 14693195. doi:10.1080/0264041031000140545.
- ^ Murray R, Stofan J. Ch. 8: Formulating carbohydrate-electrolyte drinks for optimal efficacy. Maughan RJ, Murray R (编). Sports Drinks: Basic Science and Practical Aspects. CRC Press. 2001: 197–224. ISBN 978-0-8493-7008-3.
- ^ Popkin, Barry M; D'Anci, Kristen E; Rosenberg, Irwin H. Water, hydration, and health: Nutrition Reviews©, Vol. 68, No. 8. Nutrition Reviews. August 2010, 68 (8): 439–458. PMC 2908954
 . PMID 20646222. doi:10.1111/j.1753-4887.2010.00304.x (英语).
. PMID 20646222. doi:10.1111/j.1753-4887.2010.00304.x (英语).
- ^ Ostermann, Marlies; Shaw, Andrew D.; Joannidis, Michael. Management of oliguria. Intensive Care Medicine. 2023-01-01, 49 (1): 103–106. ISSN 1432-1238. PMID 36266588. doi:10.1007/s00134-022-06909-5 (英语).
- ^ Aghsaeifard, Ziba; Heidari, Ghobad; Alizadeh, Reza. Understanding the use of oral rehydration therapy: A narrative review from clinical practice to main recommendations. Health Science Reports. September 2022, 5 (5): e827. ISSN 2398-8835. PMC 9464461
 . PMID 36110343. doi:10.1002/hsr2.827 (英语).
. PMID 36110343. doi:10.1002/hsr2.827 (英语).
- ^ Kim, Soo Wan. Hypernatemia : Successful Treatment. Electrolyte & Blood Pressure. 2006, 4 (2): 66–71. ISSN 1738-5997. PMC 3894528
 . PMID 24459489. doi:10.5049/EBP.2006.4.2.66 (英语).
. PMID 24459489. doi:10.5049/EBP.2006.4.2.66 (英语).
- ^ Tinawi, Mohammad. New Trends in the Utilization of Intravenous Fluids. Cureus. 2021-04-21, 13 (4): e14619. ISSN 2168-8184. PMC 8140055
 . PMID 34040918. doi:10.7759/cureus.14619
. PMID 34040918. doi:10.7759/cureus.14619  (英语).
(英语).
- ^ Hall, John E.; Hall, Michael E.; Guyton, Arthur C. Guyton and Hall textbook of medical physiology 14th. Philadelphia, PA: Elsevier. 2021. ISBN 978-0-323-67280-1.
- ^ Gawronska, Julia; Koyanagi, Ai; López Sánchez, Guillermo F.; Veronese, Nicola; Ilie, Petre Cristian; Carrie, Anne; Smith, Lee; Soysal, Pinar. The Prevalence and Indications of Intravenous Rehydration Therapy in Hospital Settings: A Systematic Review. Epidemiologia. 2022-12-31, 4 (1): 18–32. ISSN 2673-3986. PMC 9844368
 . PMID 36648776. doi:10.3390/epidemiologia4010002
. PMID 36648776. doi:10.3390/epidemiologia4010002  (英语).
(英语).
- ^ Ellershaw JE, Sutcliffe JM, Saunders CM. Dehydration and the dying patient. Journal of Pain and Symptom Management. April 1995, 10 (3): 192–197. PMID 7629413. doi:10.1016/0885-3924(94)00123-3
 .
.
- ^ El Khayat, Moussa; Halwani, Dana A.; Hneiny, Layal; Alameddine, Ibrahim; Haidar, Mustapha A.; Habib, Rima R. Impacts of Climate Change and Heat Stress on Farmworkers' Health: A Scoping Review. Frontiers in Public Health. 2022-02-08, 10. ISSN 2296-2565. PMC 8861180
 . PMID 35211437. doi:10.3389/fpubh.2022.782811
. PMID 35211437. doi:10.3389/fpubh.2022.782811  .
.
- ^ Bruno, Chevonne; Collier, Annaleise; Holyday, Margaret; Lambert, Kelly. Interventions to Improve Hydration in Older Adults: A Systematic Review and Meta-Analysis. Nutrients. 2021-10-18, 13 (10): 3640. ISSN 2072-6643. PMC 8537864
 . PMID 34684642. doi:10.3390/nu13103640
. PMID 34684642. doi:10.3390/nu13103640  (英语).
(英语).
- ^ Canavan, Amy; Billy S. Arant, Jr. Diagnosis and Management of Dehydration in Children. American Family Physician. 2009-10-01, 80 (7): 692–696. PMID 19817339 (美国英语).
参考书籍
[编辑]- Byock I. Patient refusal of nutrition and hydration: walking the ever-finer line. The American Journal of Hospice & Palliative Care. 1995, 12 (2): 8, 9–8,13. PMID 7605733. S2CID 46385519. doi:10.1177/104990919501200205.
- Schoeller, Dale A. Hydrometry. Heymsfield, S. (编). Human Body Composition. Human Kinetics. 2005 [2025-01-24]. ISBN 978-0-7360-4655-8.
- Steiner MJ, DeWalt DA, Byerley JS. Is this child dehydrated?. JAMA. June 2004, 291 (22): 2746–2754. PMID 15187057. doi:10.1001/jama.291.22.2746.
